In recent months one thought has been occurring to be regarding classification of Visual Impairment and blindness.
ddd
ddd
I find it is strange that the most widely understood classification of blindness and visual impairment in surveys do not have complete grounding in ICD-10/ ICD-11. As you will see below, nowhere is “Better Eye” visual acuity mentioned. But the same can be interpreted. For monocular codes, the worse affected eye is being considered and the other eye has to be better. So it can be interpreted that for binocular codes, the better eye is considered and other eye will have to be worse.
There has been a change in global definitions of Blindness and Visual Impairments globally over the years. These are summarised in the World Report on Vision (page 12) and reproduced below.
It is interesting that the World Report on Vision differentiates between how VI is classified and how it is reported/measured in surveys.
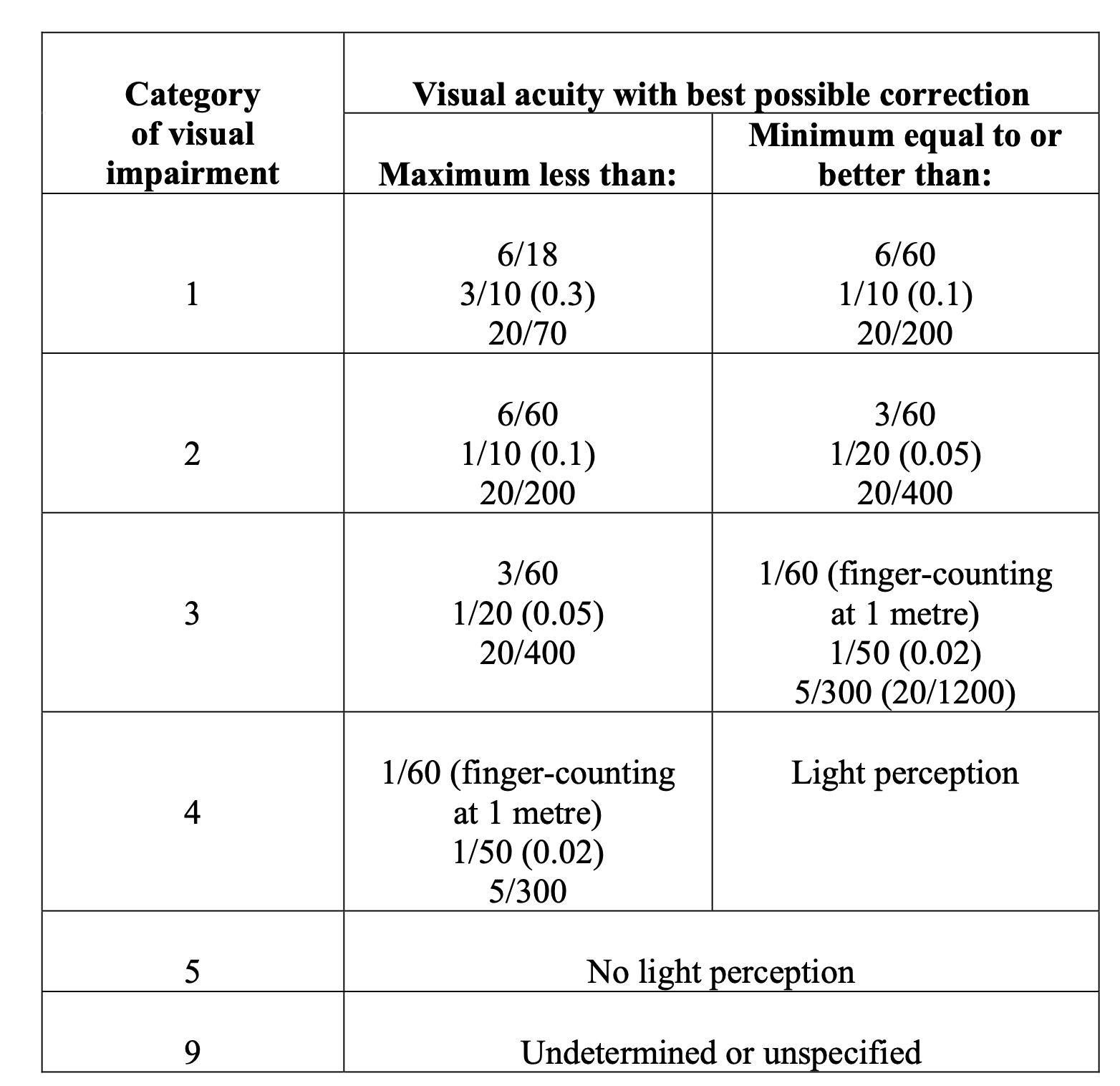
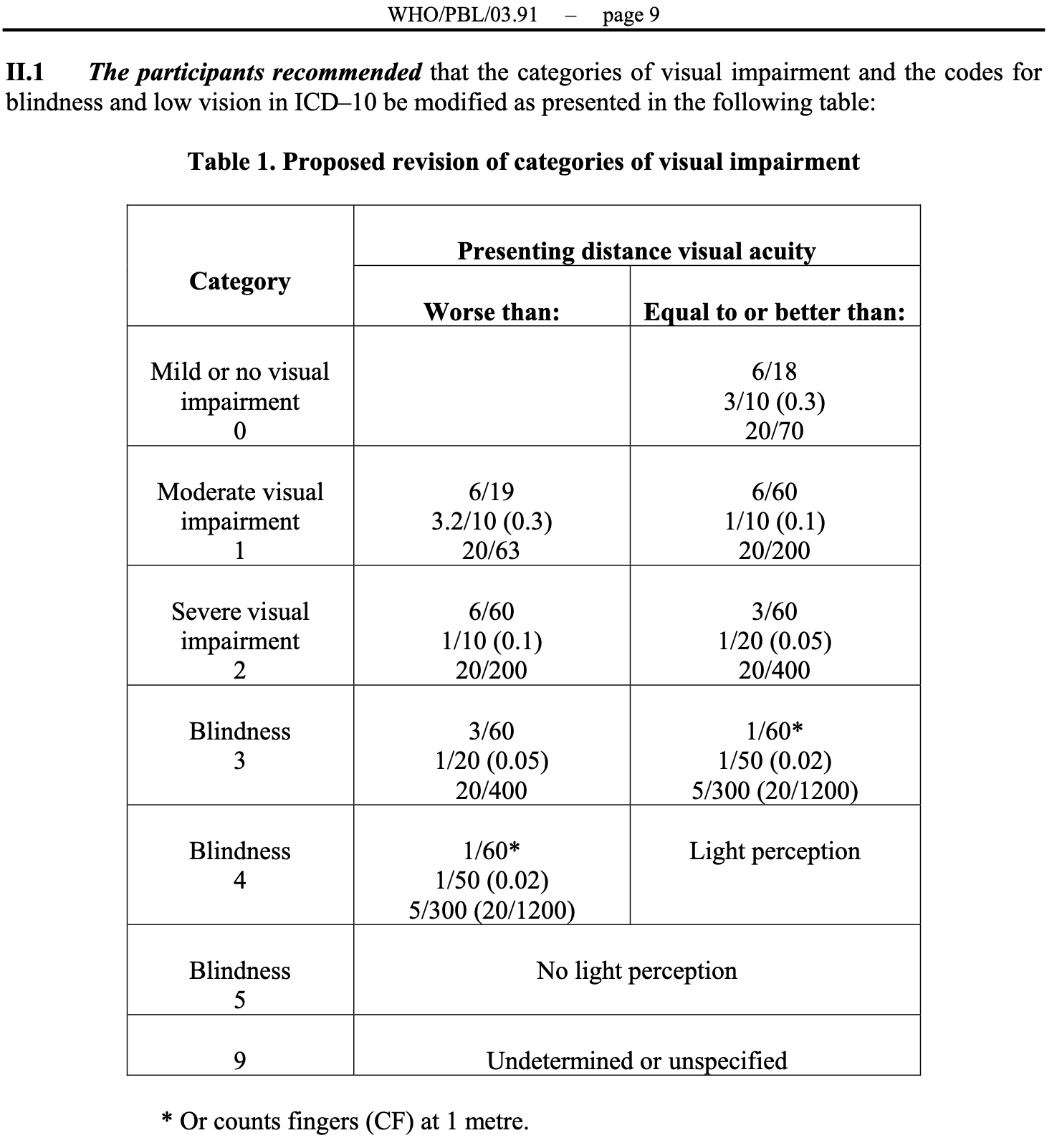
Box 1.3. Evolution of the classification of vision impairment
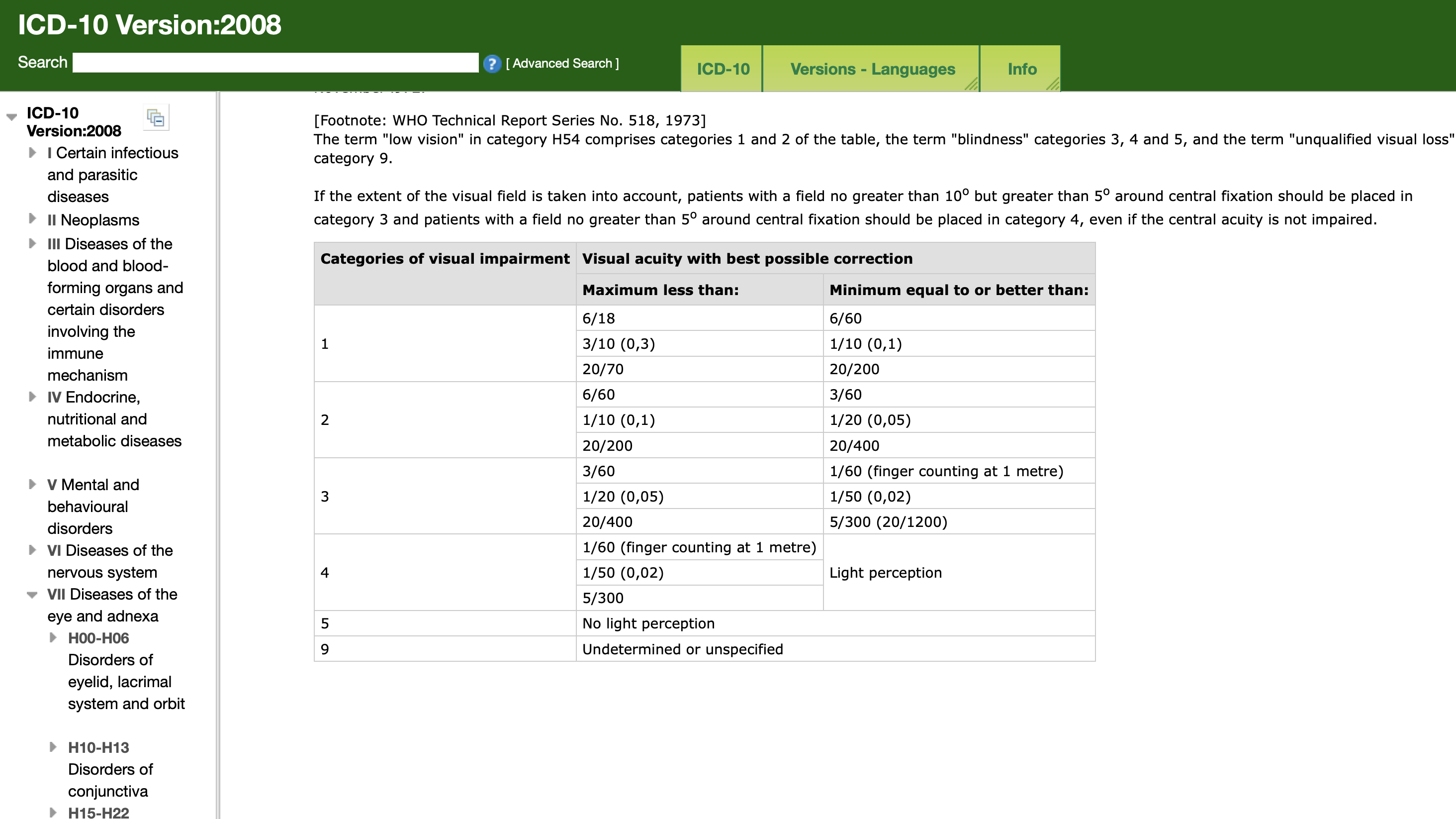
The classification of vision impairment using visual acuity has changed over time:
— In 1972, a WHO study group established categories of vision impairment and blindness in order to facilitate the collection of population-based data in a uniform format. At that time, the prevalence of vision impairment was calculated based on best-corrected (i.e. tested with spectacles if usually worn, or a pinhole) in the better eye. The cut-off for categorizing vision impairment was a best-corrected visual acuity of less than 6/18, while blindness was categorized as a best-corrected visual acuity of less than 3/60.
— In 2010, the classification of vision impairment was updated based on the premise that (i) the use of “best corrected” visual acuity overlooks a large proportion of people with vision impairment due to uncorrected refractive error; and (ii) there was no distinction between those who have varying levels of blindness (e.g. no perception of light and those that have light perception but still measure less than 3/60 in the better eye). As a result, “best-corrected” visual acuity was replaced with “presenting” visual acuity (i.e. the visual acuity of a person as she or he presents to the examination); blindness was further subcategorized into three distinct levels of severity.
— Recently, some investigators have adopted a more stringent cut-off for categorizing vision impairment (i.e. a visual acuity of less than 6/12 in the better eye) in recognition of a growing body of evidence that milder reductions in visual acuity impacts every day functioning of individuals.
Box 1.4 Changing the way vision impairment is reported
The measure of vision impairment typically reported in population-based surveys is based on visual acuity in the better eye of a person as presented in examination. If spectacles or contact lenses are worn – for example to compensate for vision impairment caused by a refractive error – visual acuity is measured with the person wearing them; thus they will be categorized as not having a vision impairment.
Measuring “presenting visual acuity” is useful for estimating the number of people who need eye care, including refractive error correction, cataract surgery or rehabilitation. However, it is not appropriate for calculating the total number of people with vision impairment. For this reason, the term “presenting distance vision impairment” is used in this report, but only when describing previous published literature that defines vision impairment based on the measure of “presenting visual acuity”.
To calculate the total number of people with vision impairment, visual acuity needs to be measured and reported without spectacles or contact lenses.
Consultation 2003
CONSULTATION ON DEVELOPMENT OF STANDARDS FOR CHARACTERISATION OF VISION LOSS AND VISUAL FUNCTIONING – https://iris.who.int/handle/10665/68601
Current Criteria
Proposed Criteria
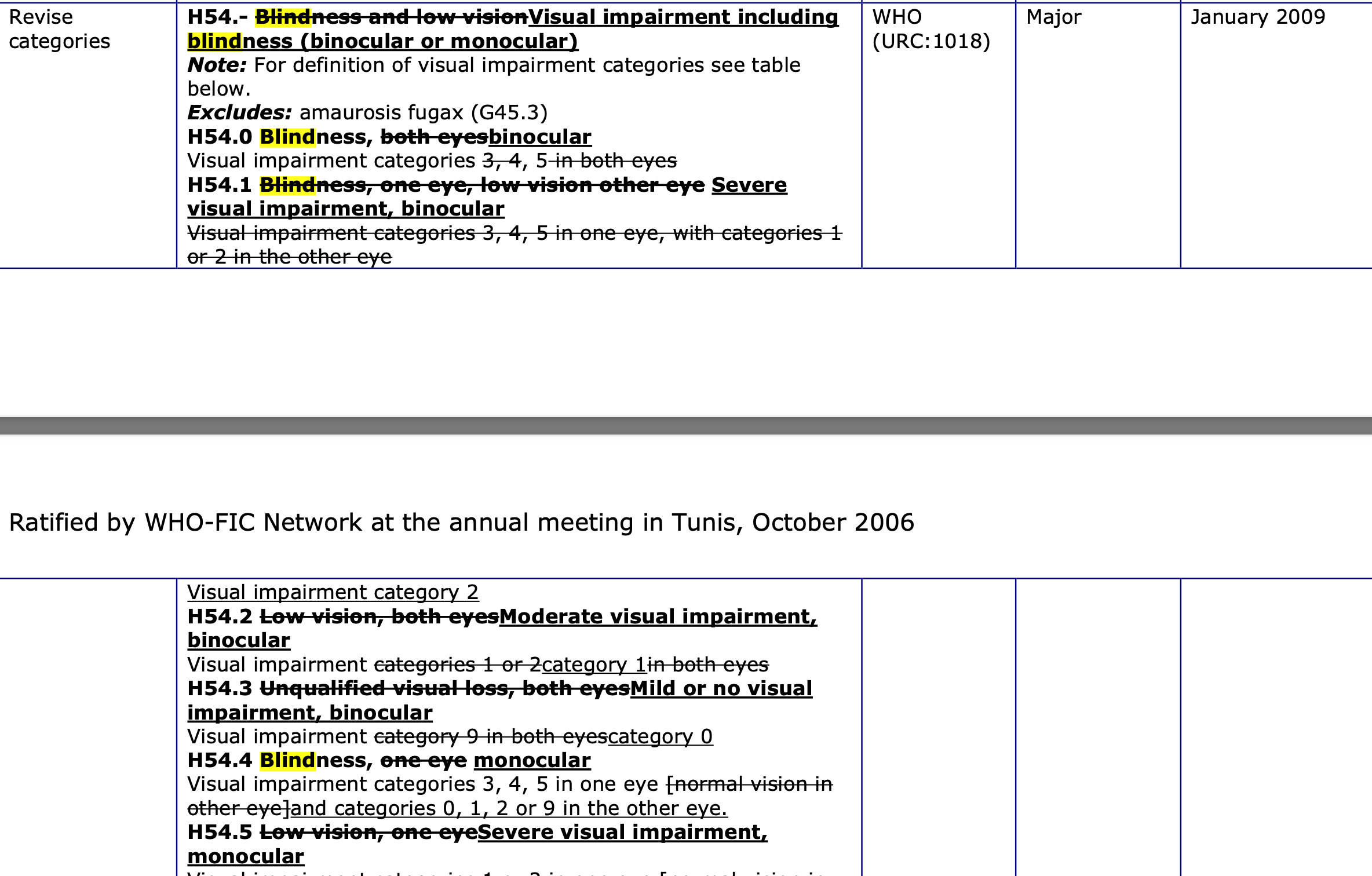
For characterizing visual impairment for codes H54.0 to H54.3, visual acuity should be measured with both eyes open with presenting correction if any. For characterizing visual impairment for codes H54.5 to H54.7, visual acuity should be measured monocularly with presenting correction if any.
ICD-10 – 2008 Version Online
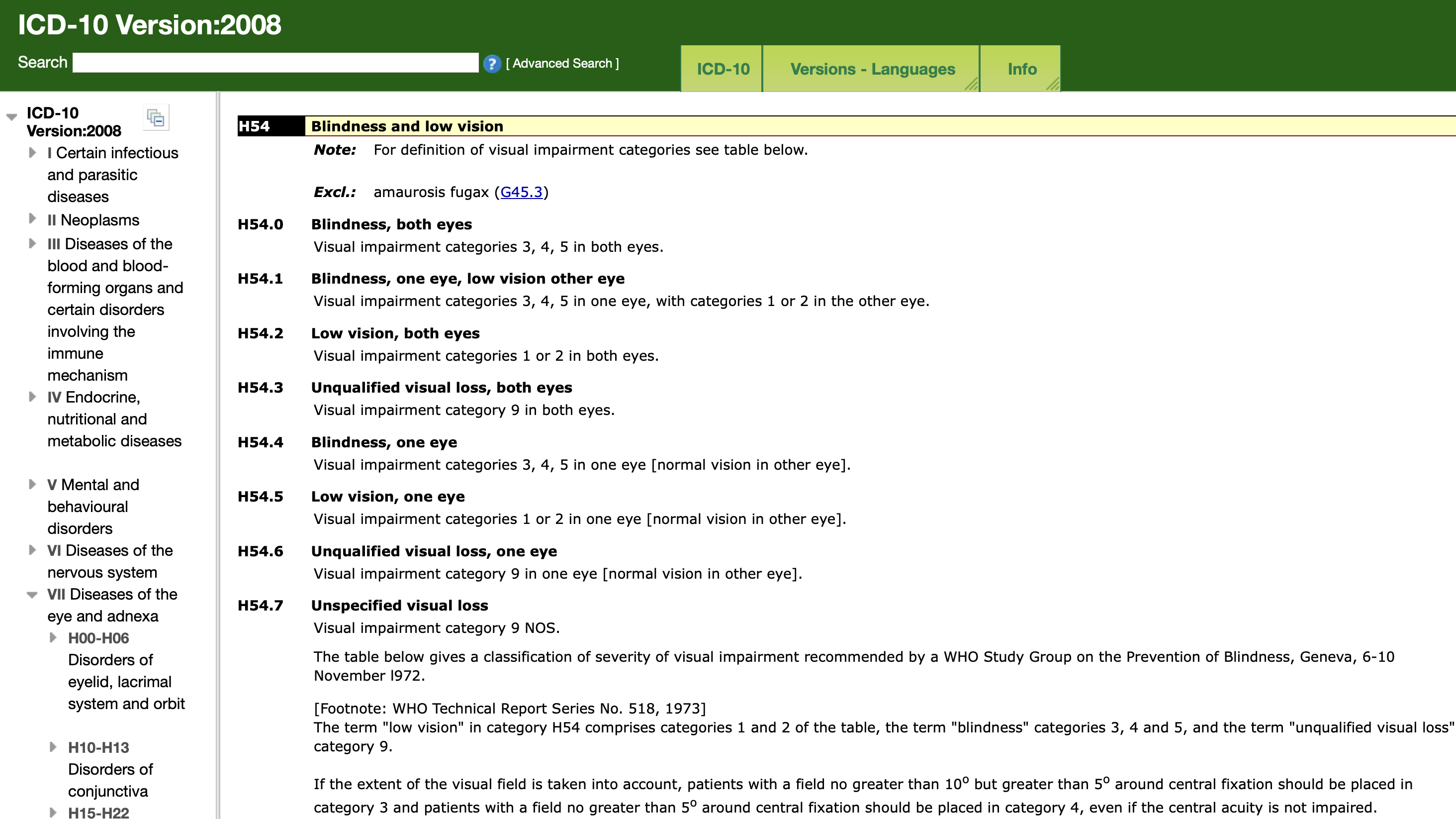
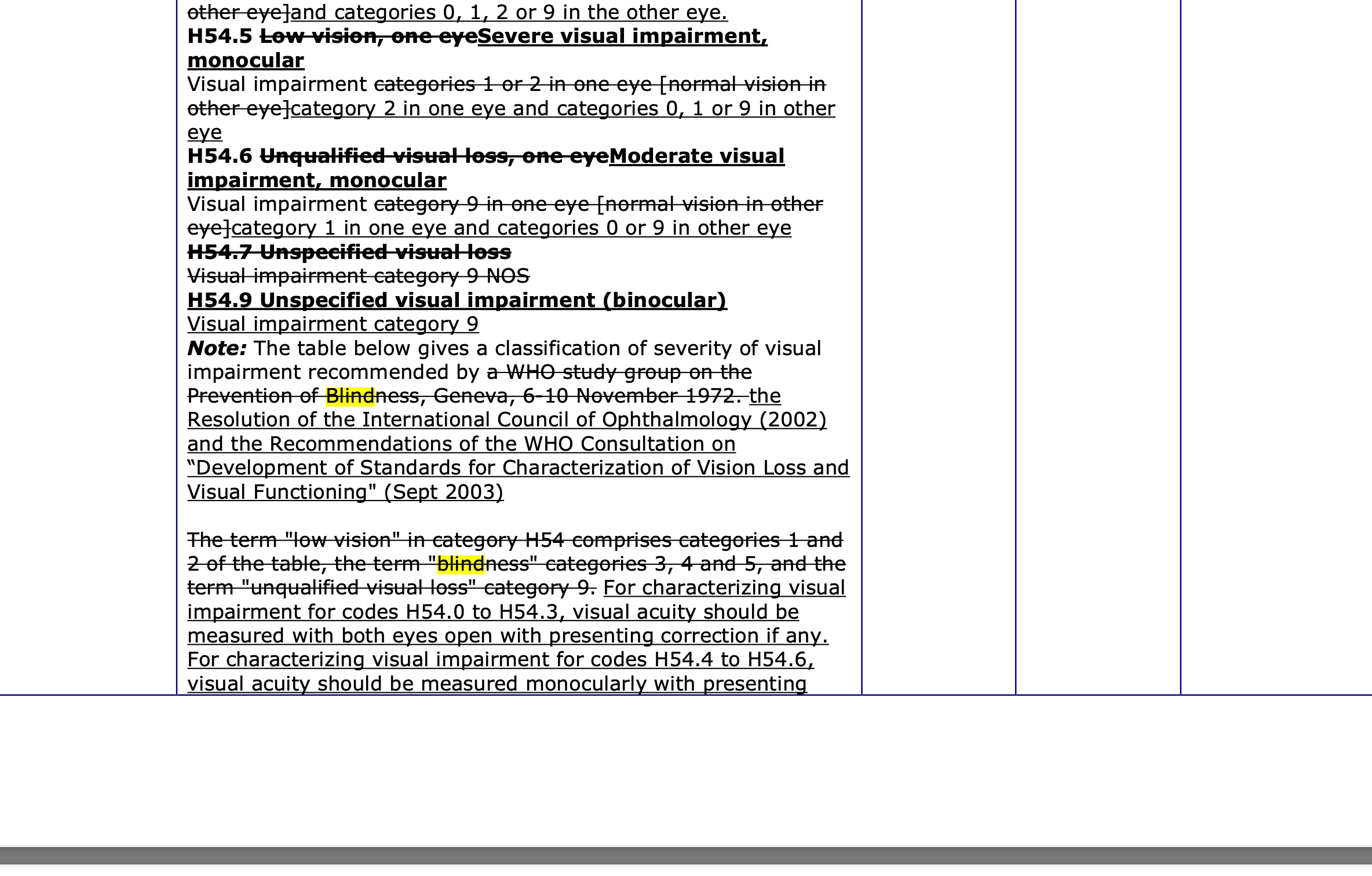
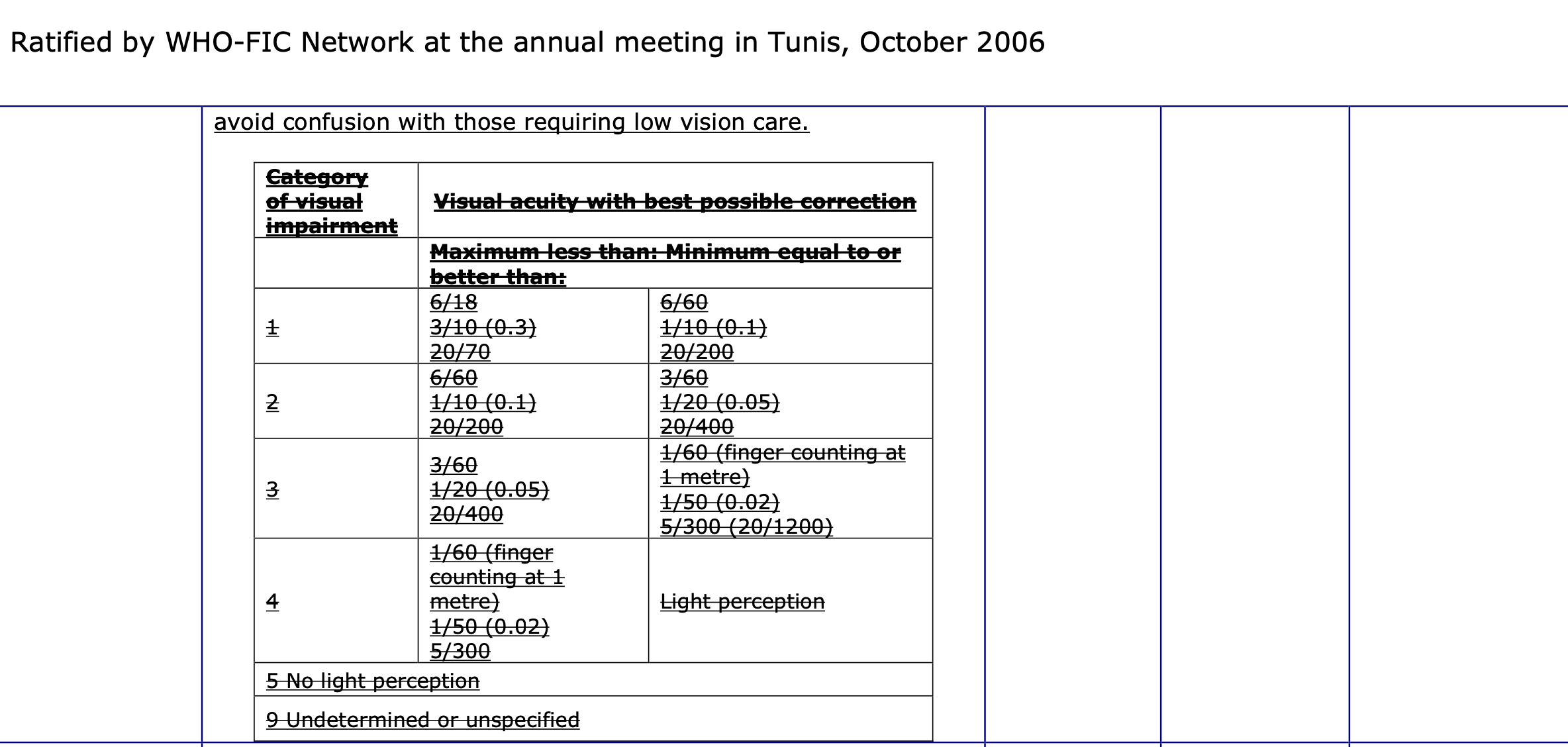
Updates in 2006

ICD-10 Version 2010 till version 2019
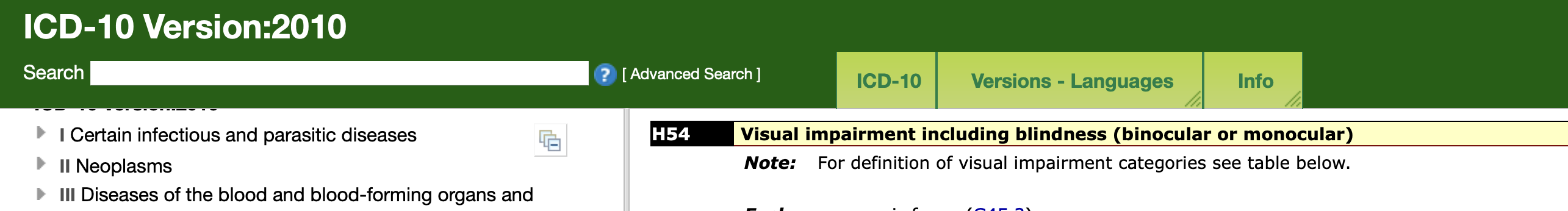

The table below gives a classification of severity of visual impairment recommended by the Resolution of the International Council of Ophthalmology (2002) and the Recommendations of the WHO Consultation on “Development of Standards for Characterization of Vision Loss and Visual Functioning” (Sept 2003).
For characterizing visual impairment for codes H54.0 to H54.3, visual acuity should be measured with both eyes open with presenting correction if any. For characterizing visual impairment for codes H54.4 to H54.6, visual acuity should be measured monocularly with presenting correction if any.
If the extent of the visual field is taken into account, patients with a visual field of the better eye no greater than 10° in radius around central fixation should be placed under category 3. For monocular blindness (H54.4), this degree of field loss would apply to the affected eye.
Note: The term visual impairment in category H54 comprises category 0 for mild or no visual impairment, category 1 for moderate visual impairment, category 2 for severe visual impairment, categories 3, 4 and 5 for blindness and category 9 for unqualified visual impairment. The term “low vision” included in the previous revision has been replaced by categories 1 and 2 to avoid confusion with those requiring low vision care.
Please note that nowhere is “Better Eye” visual acuity mentioned. But the same can be interpreted. For monocular codes, the worse affected eye is being considered and the other eye has to be better. So it can be interpreted that for binocular codes, the better eye is considered and other eye will have to be worse.
I find it is strange that the most widely understood classification of blindness and visual impairment in surveys do no have complete grounding in ICD-10
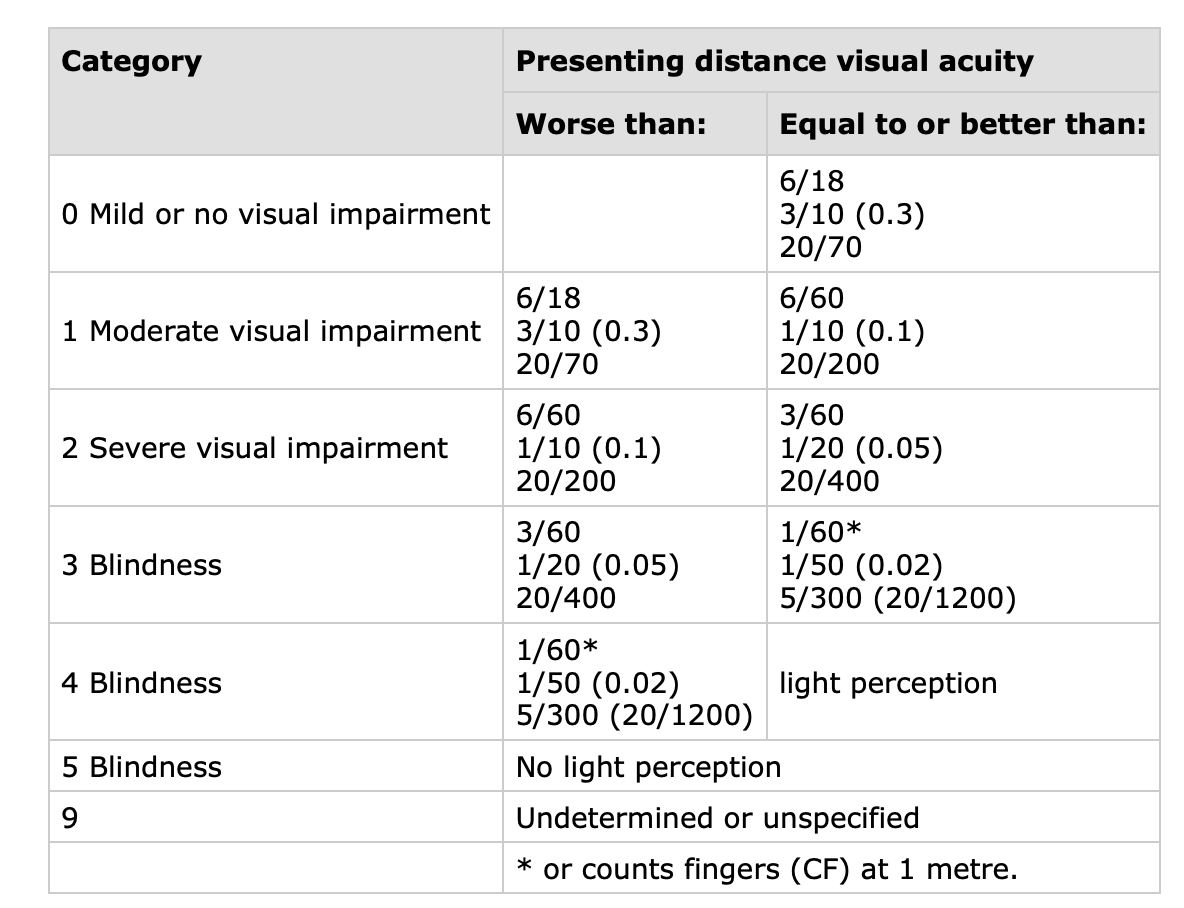
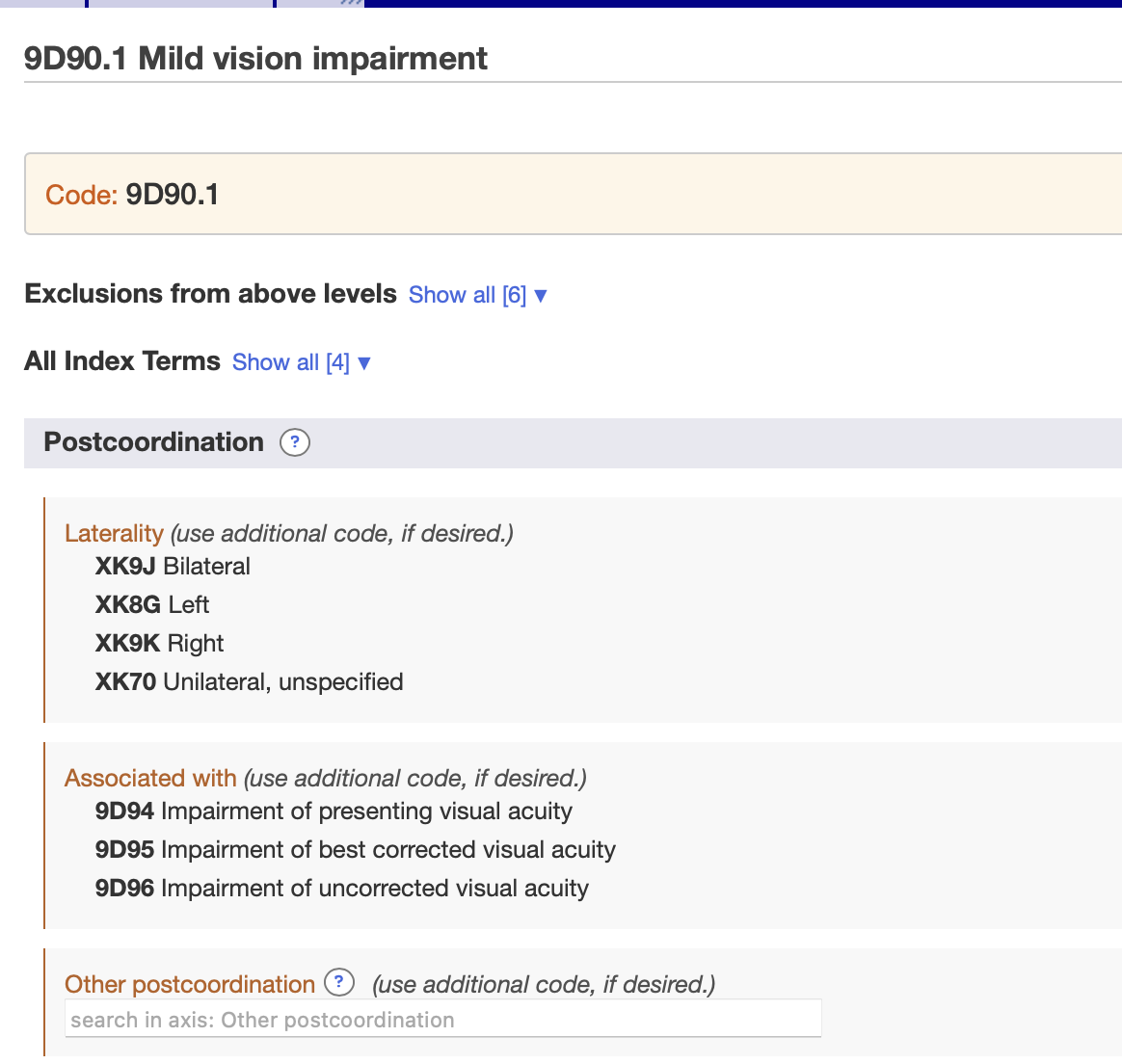
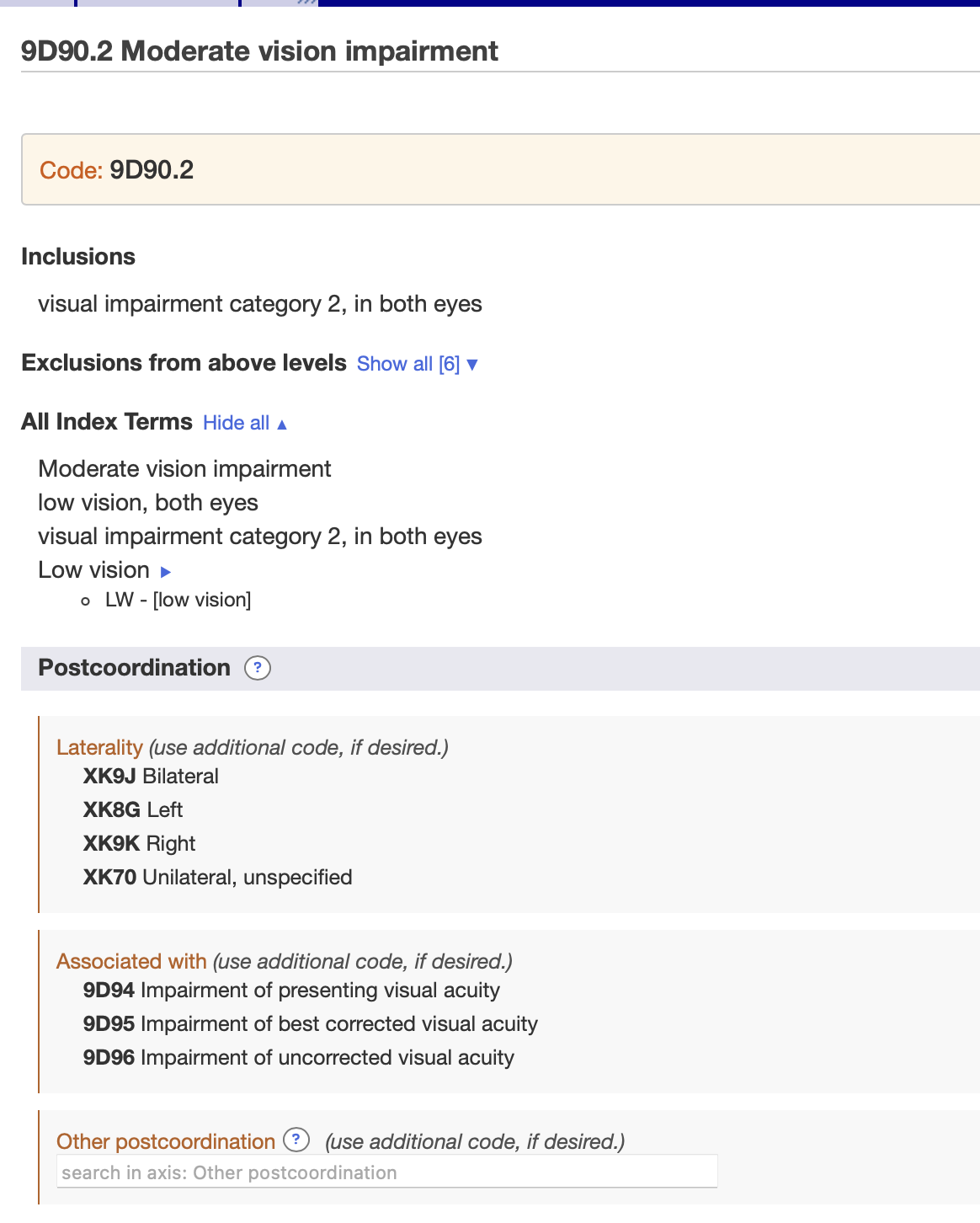
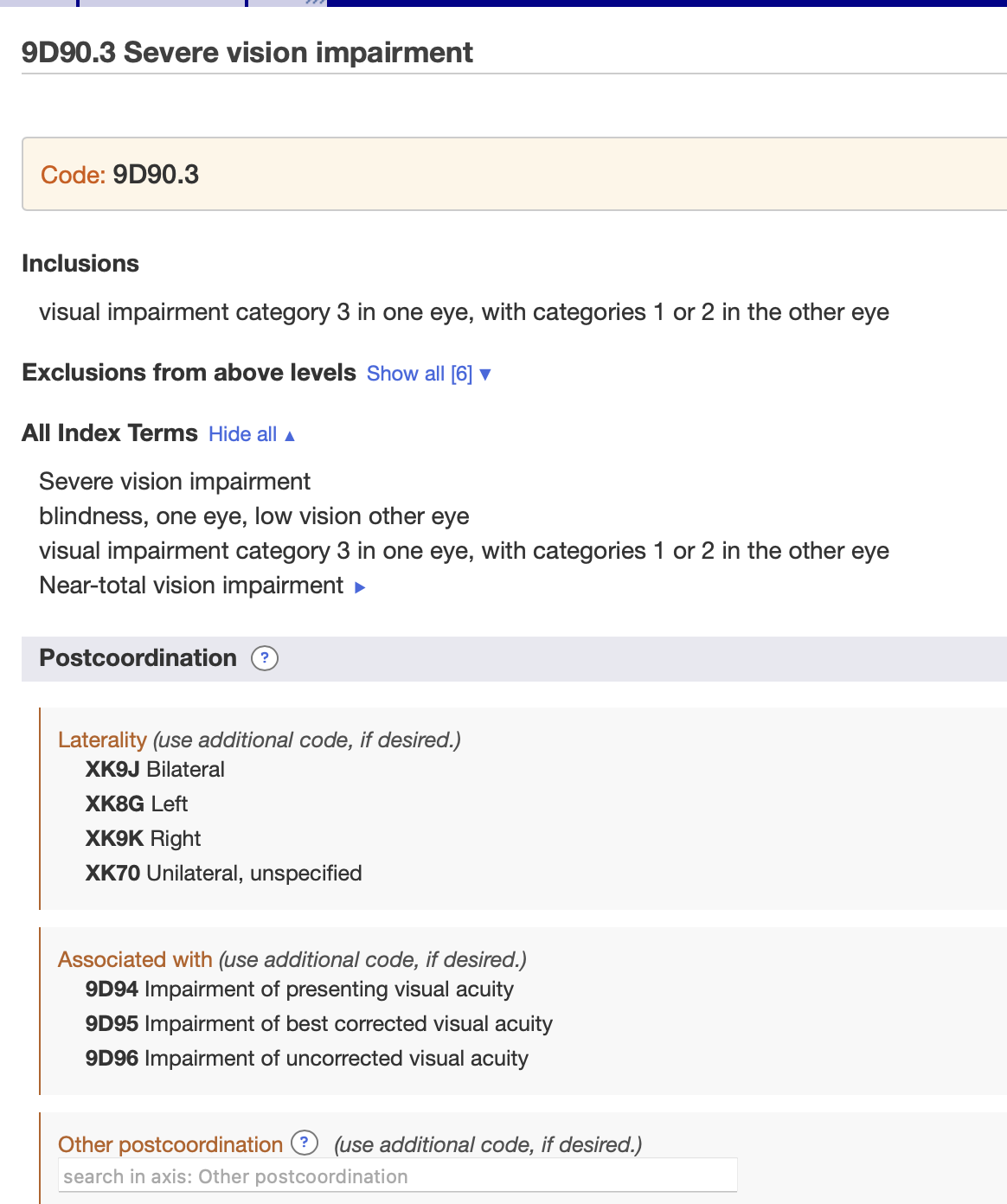
ICD-11

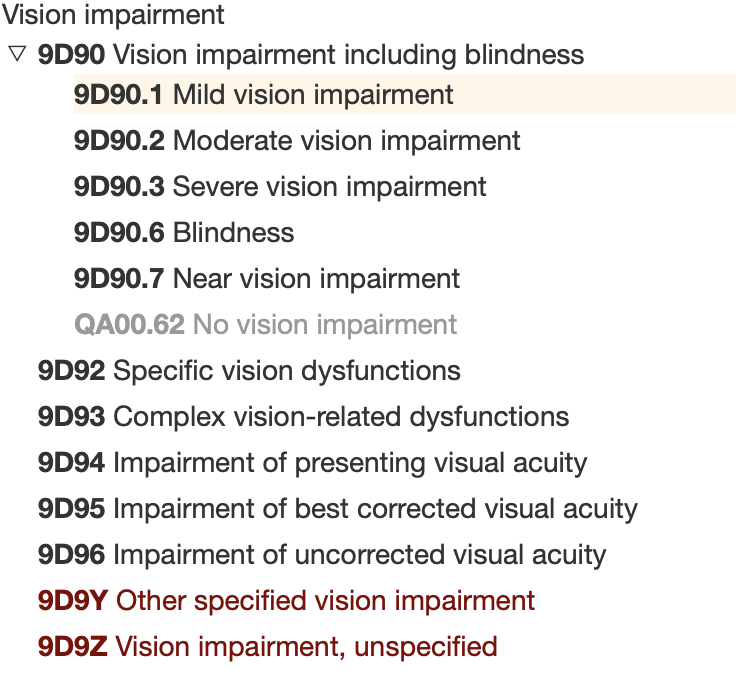
The table below gives a classification of severity of vision impairment based on visual acuity. For epidemiological studies, it is recommended to collect the following information on visual acuity for each eye, for both eyes open and for distance and near. a) Uncorrected visual acuity b) Presenting visual acuity c) Best corrected visual acuity
Blindness is also categorized according to the degree of constriction of the central visual field in the better eye to less than 10 degrees.
For capturing and coding of “No vision impairment”, use QA00.62 (QA00.6 Examination of eyes or vision).
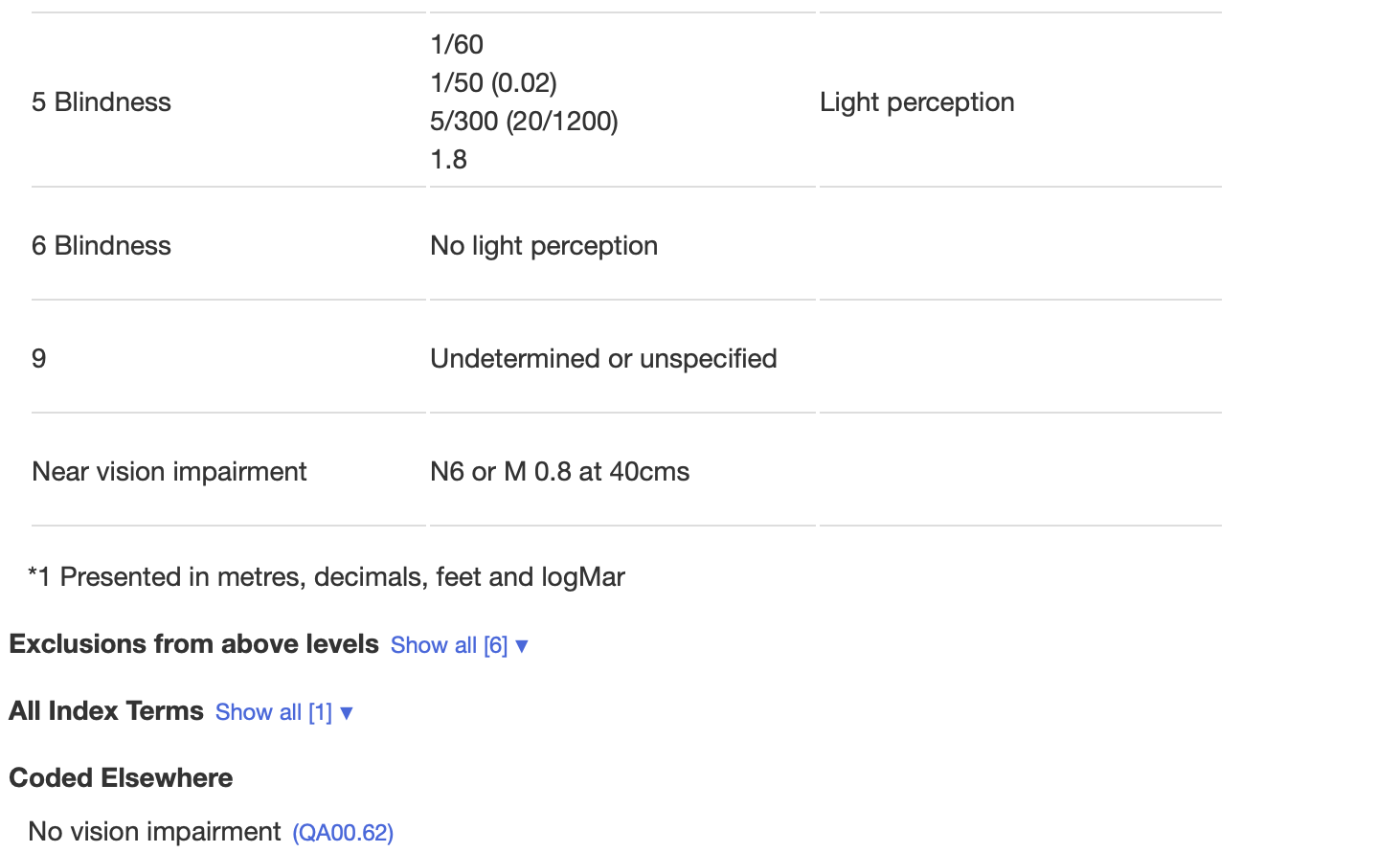
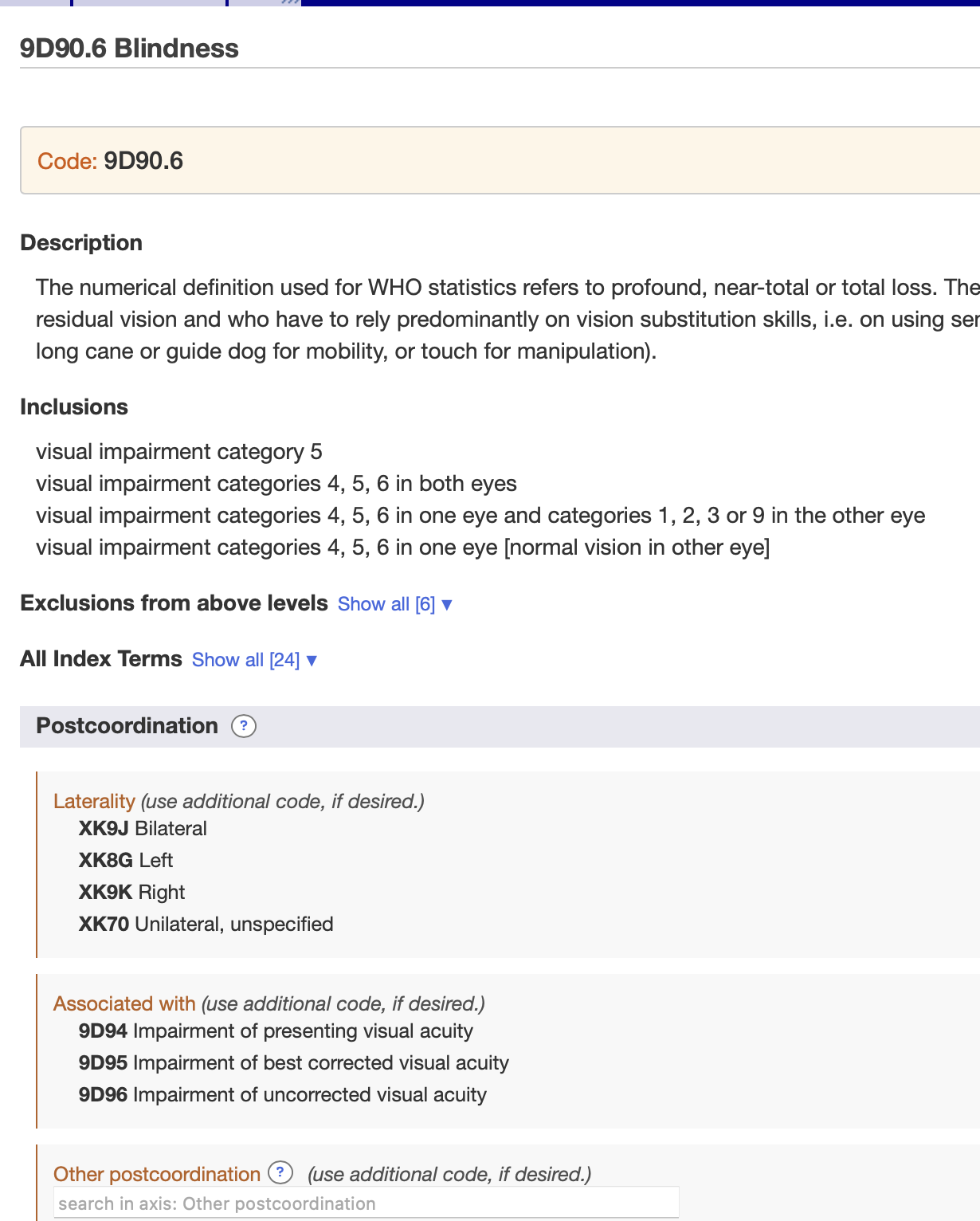
The numerical definition used for WHO statistics refers to profound, near-total or total loss. The functional definition refers to individuals who have little or no residual vision and who have to rely predominantly on vision substitution skills, i.e. on using senses other than vision (Braille or talking books for reading, a long cane or guide dog for mobility, or touch for manipulation).
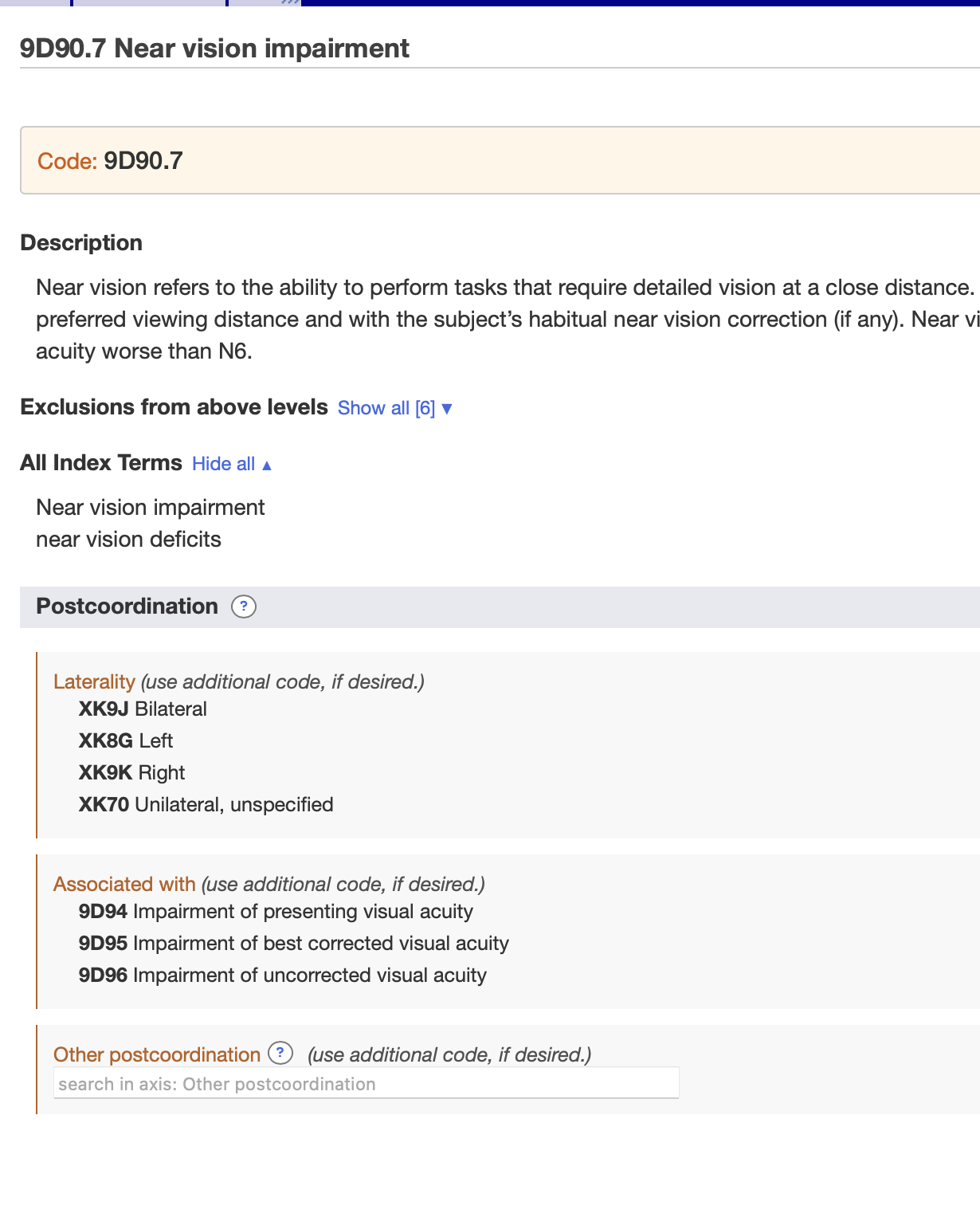
Near vision refers to the ability to perform tasks that require detailed vision at a close distance. It should be measured with both eyes open at the subject’s preferred viewing distance and with the subject’s habitual near vision correction (if any). Near vision impairment is characterised by a presenting near visual acuity worse than N6.